Before you commercialize, ask:
What is the
Reimbursement
Outlook?
Payors — a key customer segment — is critically underrepresented
in the development and launch of testing technology
• Payor input on technology acceptance and reimbursement is often seen as an afterthought or standalone function.
• Companies tend to focus on driving physician demand and do not harmonize the demand with its reimbursability.
Misaligned values and an unsynchronized approach to payors puts your test at risk of missing market and revenue expectations.
Understand the test's reimbursement outlook
• Quantify the Reimbursable Addressable Market
• Glean deep insight on prescriber relevance and their adoption journey
• Discover key market forces and trends that impact reimbursement
Improve the test's reimbursement outlook
• Get critical payor feedback and alignment upfront
• Determine minimum and ongoing evidence requirements
• Formulate demand generation strategies that drive reimbursement
create a roadmap to predictable revenue
• Harmonize reimbursement efforts with commercial strategy
• Balance predictable reimbursement with alternative paths if necessary
• Plan to manage risks and scale operations
Target your reimbursable addressable market
The reimbursable addressable market (RAM) is the portion of the total addressable market (TAM) for a clinical test that is realistically paid by insurers.
Market sizing calculation based on a proposed list price or expected payment without due diligence will overestimate the possible return of a test and mislead shareholders. The RAM takes into account the likely coverage and reimbursement to generate an accurate estimate of the potential market, which in turn informs the commercial strategy.
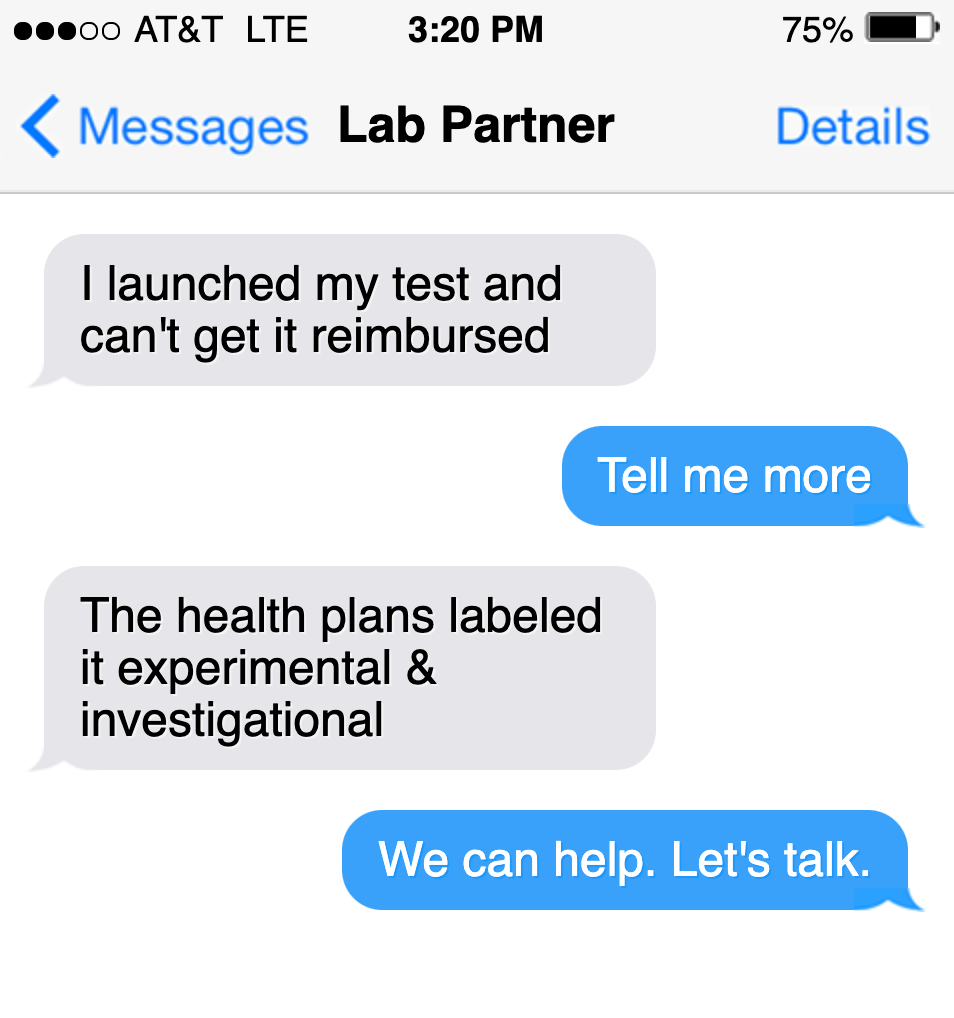
ROUTE TO REIMBURSEMENT RECOVERY
Integration of the reimbursement model during early stages of test development is most effective as it aligns the test with the shortest and most likely path towards profitability. However, not all commercialized tests will have integrated the model early in the process.
The principles of The Reimbursement Model can be retooled to help reverse unfavorable payor outcomes such as ‘experimental & investigational’ designations in medical policy and/or poor average sales pricing that mirrors undifferentiated technology.